

It was also referred to as “basilarization” one of the ICVA by Caplan ( 9).Īlthough the existence of PICA-VA is known, relatively little information has been revealed from clinical studies regarding its prevalence and relationship to vertebrobasilar stroke. This type of variation is termed a vertebral artery terminated in PICA (PICA-VA) ( 6– 8). One less common variation of VA is that a hypoplastic VA does not unite with the contralateral VA but ends into the PICA. The posterior inferior cerebellar artery (PICA) is a principal branch of the VA and has no alternative collateral circulation ( 5). In recent years, evidence has been raised that VAD is an independent risk factor for posterior circulation ischemic stroke ( 1– 4). Thus, traditionally VADs have traditionally been regarded as a normal congenital vascular variant of VAs.
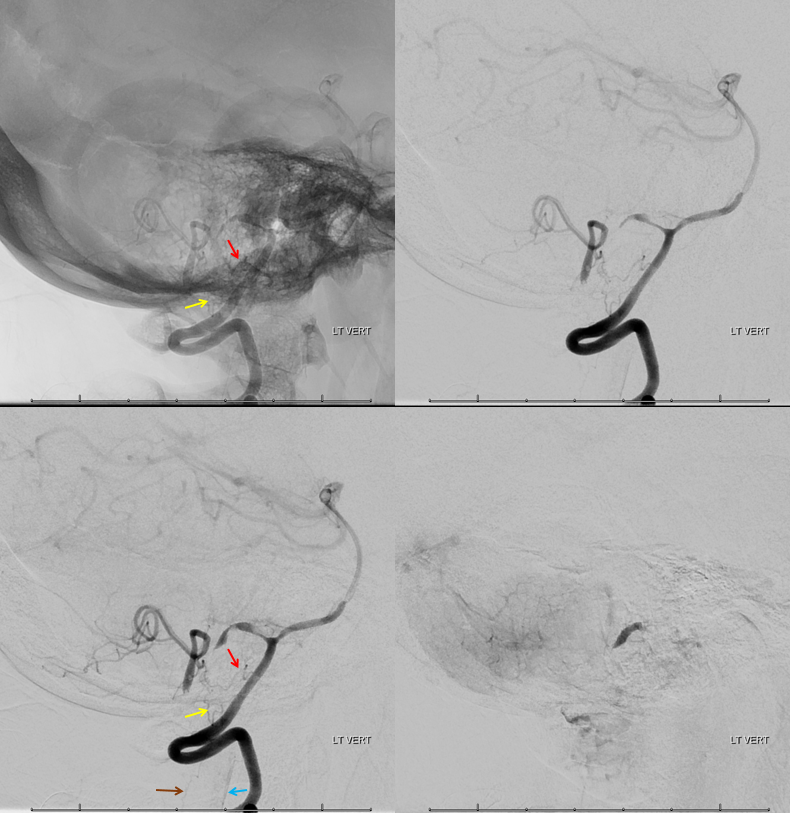
In most conditions, if a VA union occurs, the non-dominant VA is likely to obtain sufficient blood supply from the dominant one. Although without a standard definition, VAD refers to the obvious asymmetry of the vertebral artery diameters on both sides ( 1). Vertebral artery dominance (VAD) is an extremely common variation of VAs. The diameters of both VAs are generally asymmetrical. The vertebral arteries (VAs) originate from the subclavian artery, and the two VAs converge to form the BA at the lower margin of the junction of the medulla oblongata and the pons. PICA-VA was an independent risk for vertebrobasilar stroke after being adjusted for a history of intracranial hemorrhage, diabetes, body mass index, and triglyceride.Ĭonclusion: The present study showed that 3.76% of patients with acute stroke had PICA-VA, which independently increased the risk of acute vertebrobasilar stroke. The prevalence of vertebrobasilar stroke was considerably higher in patients with PICA-VA than those without (40.2%, 37/92 vs. Among them, 95 patients (3.76%, 95/2,528) had the variation of PICA-VA, 51 of which (53.7%) were located on the right side. Results: From 1 August 2015 to, a total of 2,528 patients were enrolled in the present study. We observed the prevalence of PICA-VA and identified a relationship between PICA-VA and vertebrobasilar stroke. PICA-VA is termed as a vertebral artery that does not communicate with the basilar artery but terminates in an ipsilateral PICA. Patients were enrolled for cerebral MRI and MRA within 1 week of stroke onset. Methods: This was a multicenter hospital-based cross-sectional study. In the present study, we aimed to investigate the prevalence and clinical significance of PICA-VA. Objective: Intracranial vertebral artery terminated in the posterior inferior cerebellar artery (PICA-VA) is the most popular variant of the posterior inferior cerebellar artery, while its prevalence and clinical significance remained unclear. 4Department of Neurology, Wuxi People's Hospital, Wuxi, China.3Department of Neurology and Stroke Center, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China.2Department of Neurology, The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, China.1Department of Neurology, The First Affiliated Hospital of Soochow University, Suzhou, China.Juehua Zhu 1 †, Ruiyun Huang 2 †, Kaiwen Ye 2, Hongbing Chen 3, Zheng Dai 4 and Yongjun Jiang 2 *


 0 kommentar(er)
0 kommentar(er)
